As seen in Psychology Today.
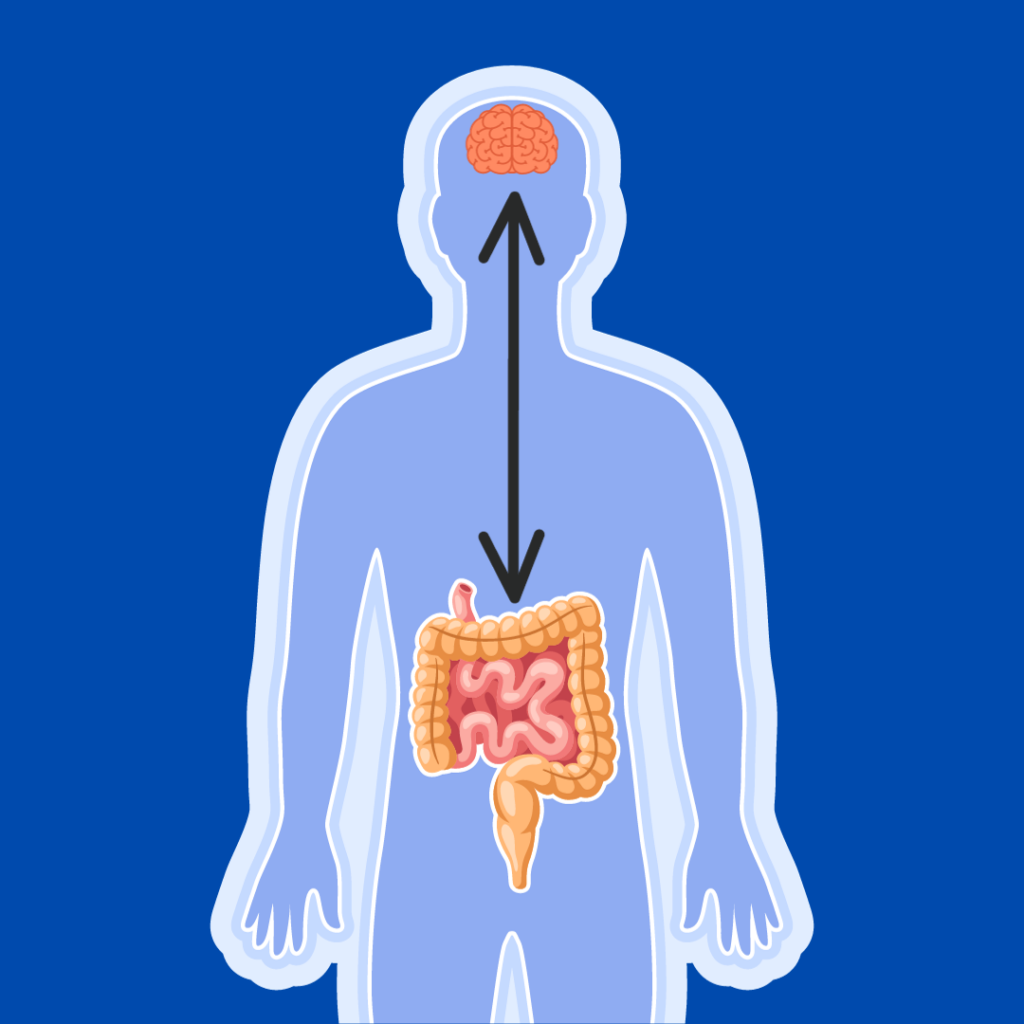
Diet and gut health are an essential core of mental health. Similarly, the gut-brain axis has progressed from an esoteric concept to a regular feature in articles about mental health in major publications like the New York Times and Washington Post.
While there is intense interest in how food affects mood and the health of the gut biota can impact the health of the brain, there seems to be less discussion of how therapies devised by psychiatrists and psychologists might resolve issues affecting the gut. I believe that is going to change.
The Gut-Brain Axis
The body’s nervous system is an enormous two-way highway that connects the central nervous system (CNS) with the peripheral nervous system (PNS). The brain is the seat of the CNS, while the PNS is an expansive network that spreads across the rest of the body. The largest component of the peripheral nervous system is the enteric nervous system (ENS), which is made up of around 200-600 million nerve cells that run from the esophagus to the anus. These nerve cells include neurons, which relay electrical and chemical messages between one another, and glia, which are the support cells for neurons—providing them with oxygen and nutrients, holding them in place and ensure they remain insulated from another, and clearing pathogens and debris. The ENS also harbors a vast gut microbiome comprised of upwards of 100 trillion microbes, including bacteria, viruses, fungi, and protozoans.
Over the last 10-15 years, researchers have become more aware of just how intimate the connection between the CNS and the ENS is, and this gut-brain axis determines how dysfunction in one system may lead to anomalies in the other. Many researchers have hoped that treating problems in the gut could lead to improvements in psychiatric symptoms, and this hope has received significant amounts of media hype, as mentioned above.
Conversely, there is significantly less interest in using stress management tools to mitigate flareups of inflammatory bowel diseases like ulcerative colitis (UC) and Crohn’s disease, despite a well-documented comorbidity of anxiety, depressive, or trauma- and stressor-related disorders. Unfortunately, psychiatry only enters the picture for IBS patients when asked to treat symptoms associated with concomitant psychiatric disorders.
Psychological Stress, Inflammation, and Gut Motility
Within the CNS, responses to psychological stresses are well characterized and involve brain regions that include the amygdala, hypothalamus, and pituitary gland, as well as the adrenal glands, which are located just above the kidneys. Known as the hypothalamic-pituitary-adrenal (HPA) axis, its activation leads to the release of stress hormones like epinephrine and norepinephrine, as well as glucocorticoids (the most well-known being cortisol). Increased HPA activity and the release of these hormones is also associated with neuroinflammation and the production of proinflammatory signaling proteins known as cytokines.
Though it’s long been recognized that stress hormones like cortisol also interact with the PNS, including the ENS, and that increases in glucocorticoids are associated with increases in gut inflammation, the exact mechanisms have been less well defined.
Until now.
With Schneider and colleagues’ aptly titled 2023 Cell paper, “The enteric nervous system relays psychological stress to intestinal inflammation,” the researchers used a mouse model to develop a clear roadmap showing how stress exacerbates intestinal inflammation and episodes of either UC or Crohn’s disease. The presence of stress-induced hormones like glucocorticoids induces specialized cells in the ENS to recruit and accumulate immune cells that produce tumor necrosis factor (TNF), a protein that causes inflammation. In other words, chronic stress effectively primes the gut for a hyperactive inflammatory response to an insult.
What is perhaps more surprising is that the presence of glucocorticoids in the ENS was associated with a delay in colonic transit time. This delay appears to be due to a decrease in mature neurons and an increase in immature (precursor-like) neurons, presumably because of increased cell death due to greater susceptibility to injury. Mature neurons are responsible for the production of acetylcholine, a neurotransmitter that is critical for muscle movements and contractions in the intestinal tract.
To put it a bit more simply, as concentrations of stress hormones accumulate in the ENS, it drives a process through which mature neurons are prematurely replaced. These prematurely replaced neurons include those that produce acetylcholine, a neurotransmitter that helps stimulate the muscles to move waste through the colon. Consequently, decrease in acetylcholine leads to delays in colonic transit times.
Finally, an investigation using human subjects found an association between stress and dysmotility, as well as an association linking elevated levels of perceived stress. This leads to increased levels of specific proteins, inflammatory markers, and inflammatory bowel disease severity. This indicates that psychological stress contributes to symptomology in those who are susceptible, and sets the stage for severe flareups of intestinal inflammation.
Reduce Stress, Reduce Inflammation
It is becoming increasingly clear that problematic inflammation doesn’t respect our neatly contrived definitions separating the CNS and PNS. As the Cell study shows, psychological stress is not merely a subjective phenomenon; it can and does have a significant impact on one’s mental health, gut health, and overall health.
If reducing the perception of stress can reduce the levels of circulating glucocorticoids, then it’s possible that psychiatry and psychology can help patients with symptom management through the use of stress mitigation techniques. These techniques may include mindfulness based stress reduction or cognitive behavior therapy, breathing exercises, yoga, massage, acupuncture, or (when appropriate) sleep therapy. In addition, use of adjunct medications when necessary may be useful. I believe more evidence will emerge showing that psychiatrists and psychologists have a larger role to play in treating inflammatory disorders, and that the Cell study is just the tip of the iceberg.
This blog was written entirely by a human with no assistance from generative AI tools.

0 Comments on "Psychiatry and Inflammatory Conditions"